In trauma leadership, things change fast — ACS standards (Orange → Gray Book), PI requirements, TQIP measures, registry updates.
You don’t know what you don’t know until you test yourself.
A quick self-check can surface blind spots before surveyors do.
1. Quiz Yourself
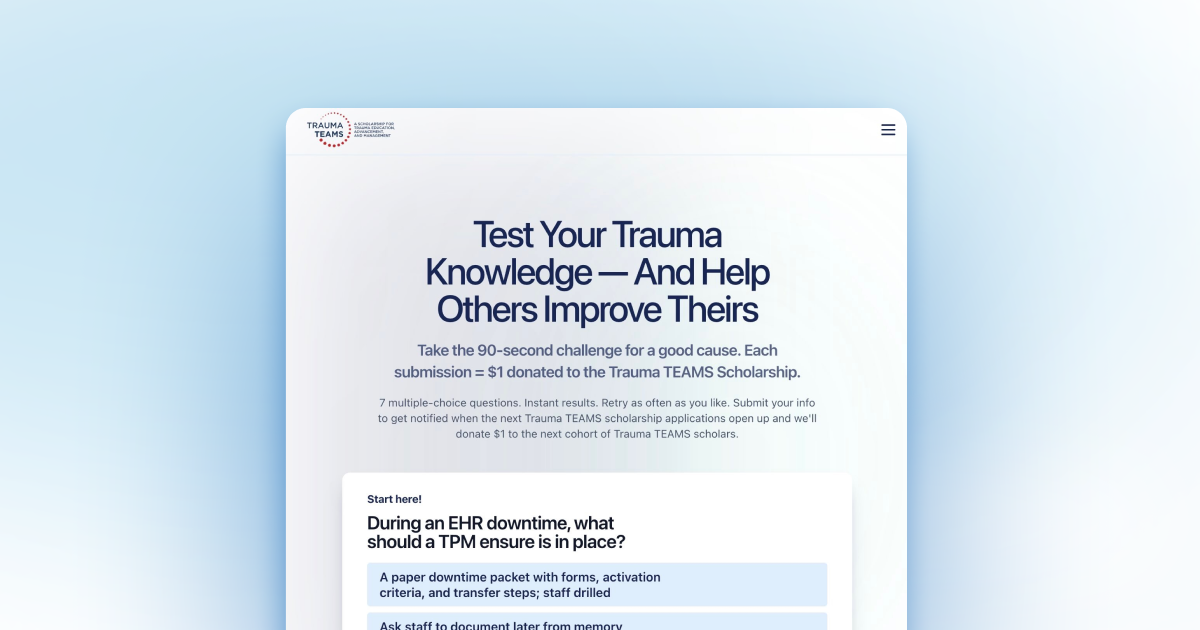
A quick quiz is a fun way to spot gaps. It’s fast, low-stakes, and sometimes eye-opening.
Instant results show where you’re solid, where you’re rusty and what the correct answers are.
Here are sample questions you might see:
- A high-acuity patient was transferred out due to lack of subspecialty coverage. What should the PI review include?
- Your trauma registry backlog is above target. What should you do first?
- How often should trauma activation criteria be reviewed and updated with stakeholders?
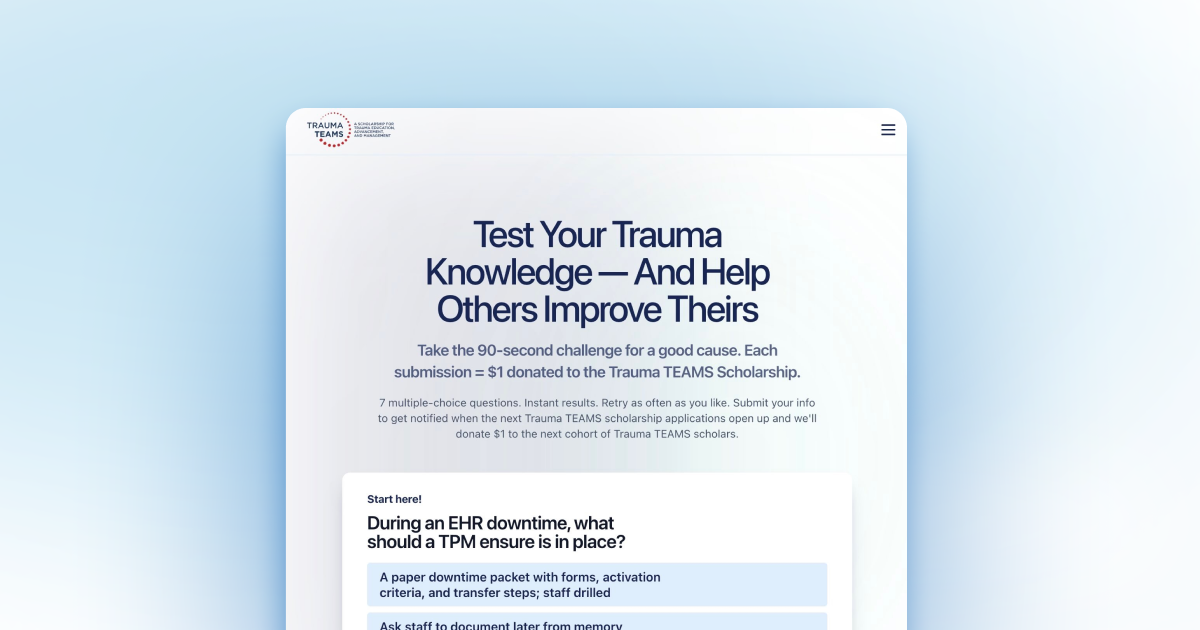
👉 Try the Trauma IQ Challenge — 7 questions, 90 seconds, instant grade, and you can retry as often as you like with new questions.
And it’s all for a good cause.
For everyone who takes the challenge and joins the Trauma TEAMS Scholarship waitlist, NQS will donate an additional $1 to the scholarship and will be notified when the next scholarship applications opens up.
2. Communicate the Core ACS Topics
ACS standards don’t cover everything a trauma leader must know, but they do spotlight the core areas surveyors look for. That focus can double as your own checklist: if the ACS is paying attention here, you should too when asking, “Do I know this?”
The topics that the ACS is focused on is just one part of what trauma leaders need to know. But they are important.
And it’s not just about knowing them. It’s:
- How do you explain the concept?
- How do you show how your program manages it?
- How do you prove it with documentation and outcomes?
PI
- Loop closure
- Event review
- Audit filters
Registry
- Abstraction standards
- IRR
- Backlog management
Triage
- Undertriage/overtriage thresholds
Education
- Documentation of attendance
- Competency
Injury prevention
- Data-driven priorities
- Measurable impact
Break These Areas Down
PI (loop closure, event review, audit filters)
Surveyors want to see that you understand the process and that your program consistently applies it (not just “we know what loop closure means,” but “here’s how we demonstrate it and track sustained improvement”).
Registry (abstraction standards, IRR, backlog)
They want assurance of accuracy, timeliness, and monitoring systems — not just that you can define IRR, but that you do IRR regularly and use it to maintain abstraction quality.
Triage (under/overtriage thresholds)
They expect you to know the thresholds and show how you measure, monitor, and address deviations in your program.
Education (attendance + competency)
They want to see proof and documentation — that your team not only attends but has competency verified.
Injury Prevention (data-driven, measurable impact)
They’ll look for evidence of alignment with trauma data and proof that your program prioritizes and measures impact, not just runs activities.
3. Communicate the PI Steps
It’s not enough to know that cases were reviewed — you should know the steps. This is about demonstrating that you understand the PI process from start to finish, not just that events were logged.
Try this: take a PI complication and walk through the steps — filter → flag → review → assign owner → loop closure. Being able to recite and explain those steps shows true leadership knowledge.
Flag → Review → Find causes → Fix with an owner + due date → Re-measure → Document loop closure (and sustain).
Example: missed VTE prophylaxis.
Can you walk through that process without notes? If you can’t, that’s a gap to close before your next verification.
When PI Steps Vary
Different complications can follow the same PI phases—flag, review, assign/fix, re-measure, close—but the owners, actions, and metrics (e.g., surgeon vs TPM, audit filters, outcome measures) vary by issue.
How do event severity and patient factors change who’s involved, what’s reviewed, and how improvement is measured?
- Higher-severity events may trigger RCA/peer review/M&M inside the Review.
- Patient type (peds vs adult) or specialty (burn, neuro, etc.) change owners, checklists, and measures, not the core phases.
Examples
The phases stay the same; the who/what/how inside each phase changes by issue.
- Missed VTE prophylaxis
- Flag: PI audit filter (missed or late VTE ppx).
- Review: contraindications, order set use, handoffs.
- Fix: add hard-stops in order set, pharmacy check, brief education.
- Re-measure: VTE ppx compliance at 30/60/90 days; VTE events.
- Close: show sustained improvement.
- CT head delay
- Flag: time-to-CT over threshold.
- Review: ED flow, transport, scanner availability, paging.
- Fix: direct-to-CT protocol, escalation pathway, scanner reserve times.
- Re-measure: median time-to-CT, % within target.
- Close: sustained metrics + adherence checks.
- Transfer delay (no subspecialty)
- Flag: transfer time > target.
- Review: recognition, consultation timing, bed search, EMTALA steps.
- Fix: pre-arranged transfer agreements, “single-call” pathway.
- Re-measure: decision-to-transfer to wheels-out.
- Close: sustained on run chart.
Now do it for other complications too, such as:
- Delayed OR for open fracture
- Inadequate documentation of alcohol screening
- Delay in antibiotic administration for open fractures
- Failed massive transfusion protocol activation
- Unplanned ICU readmission
- Missed spinal clearance
- Delay in pain management for pediatric patients
- Delayed airway management
- etc
What’s Your Score?
You don’t need a surveyor to test yourself — and you can even have a little fun doing it. Just a few minutes of honest self-checking can reveal blind spots and keep you sharp.
Start with the Trauma IQ Challenge — quick, fun, and every play helps fund future trauma leaders through the TEAMS Scholarship.