85 Trauma Performance Metrics (and how to calculate them for your dashboard)
Calculating dozens and dozens of trauma performance metrics manually each month is more than a chore; it can be a full day's work.
This necessary evil not only devours your time but also keeps you from focusing on other critical aspects of patient care and program management.
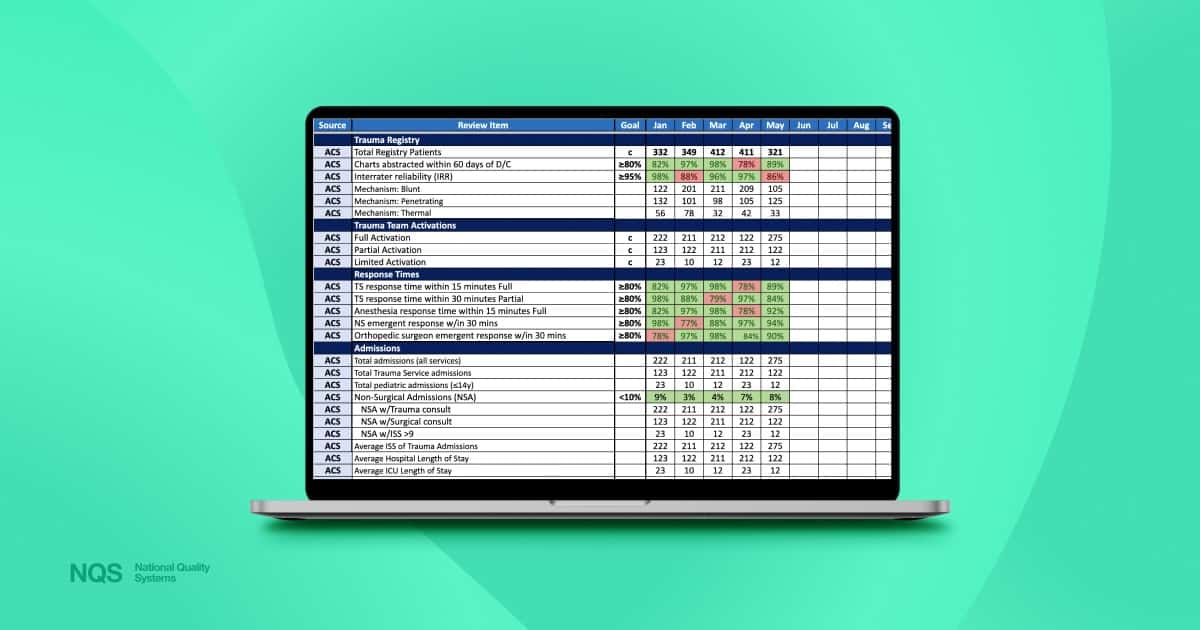
To help you streamline the tallying of the 85 most crucial trauma metrics for your dashboard, we’ve created the cheatsheet resource below. (These are the same 85 metrics we used in our free trauma dashboard excel template. We also have a video at that link that dives deeper into how to add the metrics to your dashboard.)
Note that this for the trauma teams that use manual performance dashboards. If you want an alternative to this, have a look at standalone dashboard. It's a modern dashboard built from your registry data, instantly updates when you import your data, and gives you instant, one-click drill-down reports.
But for the manual approach, let's manually tally 85 measurements…
Numerators and Denominators for Percentage Metrics
In addition to metrics needing only a simple count value, some metrics like percentages need to be calculated. Many trauma professionals grapple with tallying metrics that need a numerator and a denominator.
We've detailed the process for each relevant metric below, ensuring clarity and ease in your workflow.
OK, let’s tally some metrics!
The Metrics
Trauma Registry
Total Registry Patients:
Value: The total number of patients entered into the trauma registry within a specific time frame.
Charts abstracted within 60 days of D/C:
Denominator: The total number of discharged trauma patients.
Numerator: The number of patient charts that were abstracted and entered into the registry within 60 days of discharge (D/C).
Interrater reliability (IRR):
Value: The consistency or agreement measurement between different raters/abstractors who collect data or classify variables in the registry.
Mechanism: Blunt:
Denominator: All trauma patients.
Numerator: The number of blunt patients.
Mechanism: Penetrating:
Denominator: All trauma patients.
Numerator: The number of penetrating patients.
Mechanism: Thermal:
Denominator: All trauma patients.
Numerator: The number of thermal patients.
Trauma Team Activations
Full Activation:
Value: The count of trauma cases that met the criteria for a full trauma team activation.
Partial Activation:
Value: The count of trauma cases that met the criteria for a partial trauma team activation.
Limited Activation:
Value: The count of trauma cases that met the criteria for a limited trauma team activation.
Response Times
TS response time within 15 minutes (Level I/II) or 30 minutes (Level III) Full:
Denominator: The number of full trauma team activations.
Numerator: The number of times the trauma surgeon responded within 15 minutes (Level I/II) or 30 minutes (Level III) for full activations.
TS response time within 30 minutes Partial (or based on institution criteria):
Denominator: The number of partial trauma team activations.
Numerator: The number of times the trauma surgeon responded within 30 minutes (or based on institution criteria) for partial activations.
Anesthesia response time within 15 minutes (Level I/II) or 30 minutes (Level III)l:
Denominator: The number of emergent OR cases
Numerator: The number of times the anesthesiologist responded within 15 minutes (Level I/II) or 30 minutes (Level III) for emergent OR cases
NS emergent response within 30 minutes:
Denominator: The number of cases requiring a neurosurgical emergent response.
Numerator: The number of times the neurosurgeon responded within 30 minutes.
Orthopedic surgeon emergent response within 30 minutes:
Denominator: The number of cases requiring an orthopedic surgeon's emergent response.
Numerator: The number of times the orthopedic surgeon responded within 30 minutes.
Admissions
Total admissions (all services):
Value: The total number of admissions across all services.
Total Trauma Service admissions:
Value: The total number of admissions that were under the care of the trauma service.
Total pediatric admissions (≤14y):
Value: The total number of admissions for pediatric patients aged 14 years or younger.
Non-Surgical Admissions (NSA):
Value: The total number of trauma admissions that did not receive surgical intervention.
NSA w/Trauma consult:
Value: The number of non-surgical admissions where a trauma consult was requested.
NSA w/Surgical consult:
Value: The number of non-surgical admissions where any surgical consult was requested.
NSA w/ISS >9:
Value: The number of non-surgical admissions with an Injury Severity Score (ISS) greater than 9.
Average ISS of Trauma Admissions:
Value: The average Injury Severity Score (ISS) for all trauma admissions.
Average Hospital Length of Stay:
Value: The average length of stay in the hospital for trauma admissions.
Average ICU Length of Stay:
Value: The average length of stay in the ICU for trauma admissions.
Average Ventilator Days:
Value: The average number of days trauma patients spent on mechanical ventilation.
Transfers
In:
Value: The count of patients transferred into the facility.
Out:
Value: The count of patients transferred out of the facility to another acute care facility.
Mortality
Death:
Value: The total number of deaths among trauma patients.
Dead On Arrival:
Value: The count of patients who were dead on arrival at the facility.
Death in the ED:
Value: The count of patients who died while in the Emergency Department.
Death in the hospital:
Value: The count of patients who died during their hospital stay after admission.
Death: w/ OFI (Opportunity For Improvement):
Value: The count of deaths where there was an identified opportunity for improvement in care.
Death: w/o OFI:
Value: The count of deaths where there was no identified opportunity for improvement in care.
Autopsies (Full Autopsy/Total Deaths):
Denominator: The total number of deaths.
Numerator: The number of full autopsies performed on those deaths.
OPO Referrals:
Value: The count of referrals made to the Organ Procurement Organization (OPO).
OPO w/Donation:
Value: The count of OPO referrals that resulted in organ donation.
Donor conversion rate:
Denominator: The total number of OPO referrals.
Numerator: The number of OPO referrals that resulted in actual organ donation.
Trauma
Missed injury (excluding radiology):
Value: The count of trauma cases where an injury was missed and not identified during the initial assessment and treatment, excluding radiological misses.
Delayed diagnosis:
Value: The count of trauma cases where there was a delay in diagnosing a condition or injury.
Readmission within 30 days:
Value: The count of trauma patients who were readmitted to the hospital within 30 days of discharge.
Prehospital
Cardiac arrest PTA (Prior to Arrival):
Value: The count of trauma patients who had a cardiac arrest before arriving at the hospital.
Airway management w/GCS <8:
Value: The count of prehospital cases where airway management was provided for patients with a Glasgow Coma Scale (GCS) score of less than 8.
Emergency Department
Under-triage:
Denominator: ISS >/= 16
Numerator: ISS >/= 16 without Full or Partial TTA
Over-triage:
Denominator: ISS < 9
Numerator: ISS < 9 with Full or Partial TTA
Antibx for open long bone fx within 60 mins of arrival:
Denominator: number of open long bone fractures
Numerator: open long bone fractures with antibiotics given w/in 60 mins of arrival
ED intubation for severe TBI:
Denominator: GCS <8
Numerator: GCS <8 with intubation in the ED
Trauma flowsheet documentation compliance:
Denominator: number of TTA’s
Numerator: TTA flowsheet compliance with all elements
Massive Transfusion Protocol activated:
Value: The count of cases where the Massive Transfusion Protocol was activated
Radiology
Radiology interpretation discrepancy (misread or missed injury):
Value: The count of cases where a discrepancy was found between initial and subsequent radiology interpretations, indicating a misread or missed injury.
Timing to IR within 60 minutes (request to needle):
Value: The count of cases where interventional radiology (IR) procedures were initiated within 60 minutes of the request.
Timing to MRI:
Value: The average time from the order to the completion of an MRI scan for trauma patients.
Surgical Services
Timing to OR for emergent cases within 60 mins:
Value: The count of emergent cases where the patient was taken to the operating room within 60 minutes of decision.
Medical/Surgical/Pediatrics
Transfer to higher level of care:
Value: The count of patients who were transferred from the trauma service to a higher level of care.
Screening for ETOH with LOS >24 hrs:
Value: The count of patients with a length of stay greater than 24 hours who were screened for alcohol (ETOH) use.
Brief Intervention and Referral to Treatment for +ETOH screening:
Value: The count of patients who tested positive for alcohol use and received a brief intervention and referral for treatment.
Ortho Trauma
Isolated Hip Fracture repair within 24 hours:
Value: The count of isolated hip fracture cases where the repair was performed within 24 hours of admission.
Femur Fx Fixation within 24 hours:
Value: The count of femur fracture cases where fixation was performed within 24 hours of admission.
Open Femur Fx Fixation within 24 hours:
Value: The count of open femur fracture cases where fixation was performed within 24 hours of admission.
Open Tibia Fx Fixation within 24 hours:
Value: The count of open tibia fracture cases where fixation was performed within 24 hours of admission.
Open Tibia Fx Washout within 24 hours:
Value: The count of open tibia fracture cases where washout was performed within 24 hours of admission.
Neuro Trauma
Neurosurgeon encumbered:
Value: The count of cases where a neurosurgeon was called and engaged with a trauma patient.
Timing to ICP monitoring within 4 hrs:
Value: The count of cases where intracranial pressure (ICP) monitoring was initiated within 4 hours of indication.
Timing to craniotomy within 60 mins:
Value: The count of cases where a craniotomy was performed within 60 minutes of decision.
Timing to trach in severe TBI within 7 days:
Value: The count of severe TBI patients who had a tracheostomy within 7 days of injury.
Timing to Spinal Decompression/Stabilization within 24 hrs:
Value: The count of patients who underwent spinal decompression or stabilization within 24 hours of admission.
TQIP Hospital Events
Acute Kidney Injury (AKI):
Value: The count of trauma patients who developed acute kidney injury during their hospital stay.
Acute Respiratory Distress Syndrome (ARDS):
Value: The count of trauma patients who developed acute respiratory distress syndrome during their hospital stay.
Alcohol Withdrawal Syndrome:
Value: The count of trauma patients who experienced alcohol withdrawal syndrome during their hospital stay.
Cardiac Arrest with CPR (in hospital):
Value: The count of trauma patients who experienced cardiac arrest and received CPR while in the hospital.
Catheter-Associated Urinary Tract Infection (CAUTI):
Value: The count of trauma patients who developed a catheter-associated urinary tract infection during their hospital stay.
Central Line-Associated Blood Stream Infection (CLABSI):
Value: The count of trauma patients who developed a central line-associated bloodstream infection during their hospital stay.
Deep Surgical Site Infection:
Value: The count of trauma patients who developed a deep surgical site infection post-operatively.
Deep Vein Thrombosis:
Value: The count of trauma patients who developed deep vein thrombosis during their hospital stay.
Delirium:
Value: The count of trauma patients who experienced delirium during their hospital stay.
Extremity Compartment Syndrome:
Value: The count of trauma patients diagnosed with extremity compartment syndrome.
Myocardial Infarction (MI):
Value: The count of trauma patients who had a myocardial infarction during their hospital stay.
Pressure Ulcer:
Value: The count of trauma patients who developed a pressure ulcer during their hospital stay.
Pulmonary Embolism (PE):
Value: The count of trauma patients who developed a pulmonary embolism during their hospital stay.
Severe Sepsis:
Value: The count of trauma patients who developed severe sepsis during their hospital stay.
Stroke/CVA:
Value: The count of trauma patients who suffered a stroke (cerebrovascular accident) during their hospital stay.
Unplanned Admission to ICU:
Value: The count of trauma patients who required unplanned admission to the ICU.
Unplanned Intubation:
Value: The count of trauma patients who required unplanned intubation.
Unplanned Visit to the Operating Room:
Value: The count of trauma patients who required an unplanned visit to the operating room.
Ventilator-Associated Pneumonia (VAP):
Value: The count of trauma patients who developed ventilator-associated pneumonia.
Conclusion
While managing trauma metrics can be daunting, we've tried to help simplify at least one part of the process. With each of these core metrics defined, we hope you find that this speeds up some of your workflow.
And if you’re in need of a trauma performance dashboard, you can free trauma dashboard excel template. And if your trauma program is in need of more advanced performance tools that save significantly more time, visit mynqs.com.
Happy metric tallying.